Finding Our Way in a Foreign Land
This is a post I never imagined I would be writing. As the pandemic grew through the winter, it seemed that the thing we feared most was the idea of being in the unfortunate group of the population to become ill. Or maybe, worse, the group that perished from it. What we’ve actually experienced in our real life was not something I could have fathomed, and I’m still struggling to understand it each day.
This post also comes with a heartfelt disclaimer. My decision to share this very personal chapter of our life is not a plea for anyone’s pity. We are not seeking your sympathy.
The way I see it, I have a choice to either suffer through hardship in silence, or to use the circumstances of my life to bring light into the world. I am choosing the latter. That has always been my belief and commitment when writing about our home and life–not to simply show off the pretty “after” photos that are staged to perfection, but to share the real stories about the hard work, grit, and determination that’s inherently a necessary part of living the good life.
Not every day is rosy. And I’m grateful for that. The challenges, bitterness, and obstacles of life are what allow us to recognize when things are good, and sweet, and beautiful. We need both of these extremes to experience true fulfillment.
Also, a word to The Fixers. You are my people–I see you, and I know your heart because I’m the same way. We are the ones who are called to service and have a deep desire to make things better for those we see hurting. It is something we strive to do because we feel very deeply and cannot tolerate the suffering of others without trying our best to solve problems.
Although I know that the intention is pure and loving, I’m asking you to refrain from offering your medical advice or opinions about my condition and treatment based on your own experiences (or experiences of others you know). While working through a health challenge, it’s important to remember that every individual’s body works differently, and we all have our own unique set of circumstances. What works for one may not be right for another for a variety of reasons.
While I’m sharing quite a bit of detail in this post, I’m certainly not including every aspect of my medical history. Please know that I trust my doctors, and the choices we’re making are based on substantially more data and history than I’m including in this post. I am fortunate to have a committed and supportive team of medical practitioners (including my own sister who is an angel on Earth) who are highly educated and respected in their fields, and we are working with them to make the best choices for our family based on my own body’s needs.

HOW THIS ALL STARTED
The first week of March, I had an irritating little cough, and Rob was feeling run down and tired. I figured I was suffering from allergies after kicking up sawdust using the saw and air compressor to work on our laundry room remodel. Rob had been putting in especially long hours working that week too, and we figured he just needed to catch up on sleep.
Within a few days, Rob was seriously ill. He was coughing horribly–waking up at night gasping for air. Coughing to the point of vomiting, and then trying not to aspirate it back into his lungs while struggling to get a breath. It was terrifying for us both.
In all our years together, I have never seen him so sick. He says he’s never been that sick in his entire life.
But I still only had an annoying little cough. We couldn’t imagine a scenario where he’d caught anything especially serious, and I wasn’t sick. I am, after all, the one with the compromised immune system. If anyone in our house is going to catch a bug, it’s me. It’s always been that way.
Three days into Rob’s illness, I crashed. All of the same symptoms. A dry, unproductive, and unrelenting cough joined by mild fever, body aches, shortness of breath, and severe headache. Neither of us could talk or take a normal breath without setting off a coughing fit.
Now that we were both horribly sick at the same time, we reached out to our family doctor. Mind you, at this time in the pandemic, there was a massive shortage of testing supplies. Unless you were hospitalized, you couldn’t get tested, and even though we were very sick, we didn’t feel that we needed hospital care. We were advised to self-quarantine and call if things got worse. We used over-the-counter medicines to control fever, pain, and manage the cough as best we could, and we camped out on the sofa with blankets and Netflix.
After about three weeks, Rob was doing quite a bit better…still struggling with a lingering cough, but otherwise feeling “okay”.
I was not.
It took almost six weeks before I started to see the beginnings of improvement. Not “all better” by any means, but I could start to see a turn in how I was feeling. The cough and shortness of breath persisted, but they were far more tolerable.
About a week or so later, however, I first noticed that my heart was racing for no apparent reason, and I had chest pain every time it would happen. I dismissed it as part of “getting over an illness”. Or maybe even some kind of lingering bronchial pain from nearly two months of coughing.
Mostly, I just figured that after having been sick for so many weeks on end, there was almost definitely a certain amount of deconditioning that my body had experienced. I figured that I would get over it as I readjusted to activity and, eventually, got back into my exercise routine.
But that’s not what happened.
With each passing week, I felt a little worse. The racing heart rate, shortness of breath, and chest pains were not only not going away…it was happening more frequently and the degree of pain was getting worse.
Finally, I reached a point where the chest pain was so overwhelming severe, that I could not dismiss it. On a scale of 1 to 10, the pain was emphatically a 10. When it would strike, I was unable to speak, breathe, or think straight. It was that type of “coming out of my skin” sort of pain that is rarely felt.
I think I should add that I’m not a person to complain about pain. In fact, I’m the exact opposite. I will dismiss my experiences and find a way to explain things away. You will never find me popping a pain killer for something that aches on my body because I’d rather just drink an extra glass of water and go to bed early first. I was a farm kid who grew up in a “walk it off” kind of family where the motto was: Whatever doesn’t kill you makes you stronger.
When I’m complaining about pain, you can be certain that it is very bad.
So, one Sunday evening, I had chest pain that was so intense that I dropped to the ground on my knees, unable to breathe, and seeing stars. Rob wanted to go to the hospital, but–as further proof of my stubborn mule attitude–I said no. We’d call the doctor in the morning.
Some of you who might be medical practitioners–or, you know, just people with common sense–are probably reading this part shaking your head in disbelief of my stubbornness. You aren’t wrong. For starters, I could have been having a heart attack or pulmonary embolism (thankfully I wasn’t). I cannot stress enough the fact that no one should read this and applaud my decision to wait seeking medical care. There is nothing admirable about denying yourself care, and it’s something I have been working for years to correct in my own psychology. Please do not follow my example if you are ever in a similar situation.

WE FINALLY GO TO THE DOCTOR
(One side note…I did not drive myself to any of these appointments because dizziness has been plaguing me every time my heart races, so it wouldn’t be safe for me to drive. However, due to COVID precautions at both the clinic and hospital, Rob had to wait in the car in the parking garage each time we made a visit, sometimes for several hours. He’s such a trooper!)
The next morning, I called the doctor’s office. They told me to come in right away. My regular doc was out, but I was able to be seen by another doctor in the office providing coverage. After an exam, EKG, and blood collection, I was sent to the hospital for a chest x-ray.
Based on my exam and description of my symptoms, the doctor believed I was likely suffering from “post-viral syndrome” in the form of pericarditis and prescribed a strong anti-inflammatory. Pericarditis is an inflammation of the membrane that surrounds the heart, and it’s known to come on after viral illnesses. It causes sharp, stabbing pain in the chest, so it definitely matched my experience.
Curiously, the xray showed no signs of inflammation or fluid accumulation around the heart as is the case with pericarditis. All of the labs were perfect, too–on paper, I appeared to be the picture of health.
The next day, the doctor had me return to the hospital for a CT coronary angiogram to rule out a pulmonary embolism. For this test, you lay on a table that slides into a tube which is actually a powerful xray machine. While you’re in the tube, contrast dye is injected through an IV in your arm so that pictures can show how the blood flows through your heart/lungs/chest.
If you’ve never had one, it’s a weird experience. The dye makes your body feel incredibly hot, starting in your throat, and you feel a bit like you’re wetting your pants as it travels south throughout the body. Very bizarre!
When this test was complete and I got up from the table, I immediately felt like I was going to fall over. I was dizzy, short of breath, and my heart was racing, so the technician made me stay seated and brought me water to drink. The feeling passed within a couple of minutes, so they ruled out any possible allergic reaction and allowed me to leave.
The doctor called that evening to say that the test showed nothing–not even supporting the pericarditis which she suspected it might catch since this test provides better images than a regular xray. But she still felt it just had to be pericarditis based on my symptoms. It just made sense. So, she sent me back to the hospital one more time for an echocardiogram.
An “echo”, as they’re nicknamed, is basically an ultrasound of your heart. The technician uses the wand just like is done on the belly of a pregnant woman to look at a baby, but instead, it’s used on the chest to look at the heart. If there was anything going wrong in how my heart was functioning, this would see it in action.
But, it didn’t.
Once again, the test revealed nothing. My heart was functioning normally. It was the right size. There was no inflammation seen anywhere. The valves were all working properly. The amount of blood passing through the chambers was grossly normal. No arrhythmia (i.e. “abnormal heart beat”) was observed during the 20 minutes of the test.
I FEEL LIKE MAYBE I’M GOING CRAZY
At this point in the diagnostic journey, I’m starting to question my own sanity. Am I imagining the pain and the symptoms? Have I suddenly become some kind of fragile individual and overreacting to something extremely minor? Is it all in my head? Or worse, am I causing this somehow?
The doctor had no answers for what I was experiencing, but assured me she didn’t think I was crazy or making anything up. As she explained to me, the tests I was going through were to rule out some really bad things that could be associated with my symptoms–not to prove/disprove that my symptoms were happening in the first place. The goal, now, was to figure out just what exactly was happening and why.

A SECOND SET OF EYES
The next week, my regular doctor was back in the office and asked me to come in so she could examine me herself. She’s been my doctor for years, and she knows me very well–both professionally and personally. Unfortunately, she was set to retire at the end of June, but while she was still there, she wanted to make her own evaluation.
At this point, I was feeling even worse than before. The pain was happening more frequently, my heart rate just kept going up, I was having more shortness of breath, and the dizziness was really taking a toll on me.
We spent an hour talking through everything that had been going on. She pressed me to really put into words what the pain felt like when it happened, and to try to remember anything else that might have been related during those times.
Those descriptions of pain are especially tough for me. Like I mentioned before, I was raised with a “walk it off” attitude. That’s not to say that my parents didn’t provide me with adequate care–that wasn’t the case at all. But I also wasn’t coddled. I was a pretty rough and tumble kid…a bit of a tomboy who liked to play in the dirt and build tree forts…and it seems like I had perpetually skinned knees and elbows for most of my childhood.
Talking about what pain feels like is outside of my wheelhouse. I have trouble (like, a lot of trouble) putting that kind of thing into words for myself, even though I can completely understand it when I hear others articulate their own pain. My doctor knows that about me, so she very patiently pressed me over and over again to describe this or that in more detail.
Finally, she wondered if maybe the extra-strong anti-inflammatories I was taking were making things worse. They’re notoriously tough on the stomach, and we started playing with a theory that maybe–just maybe–the chest pain had nothing to do with my heart. Perhaps it was esophageal.
If you think about it, the location in the body is basically the same, so maybe I had an ulcer in my esophagus and the anti-inflammatories were actually making it worse because they were causing excess stomach acid. Maybe my heart rate wasn’t causing the chest pain–maybe the pain was causing an increase in my heart rate.
She took me off of the anti-inflammatories completely that day and prescribed a heavy-handed dose of a proton-pump inhibitor. PPIs work to shut off production of stomach acid, so if I was suffering from an ulcer, this would theoretically relieve the pain.
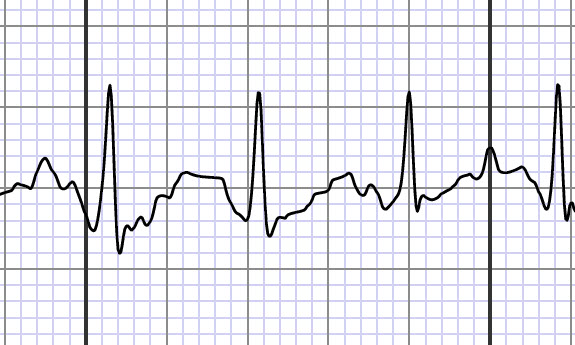
She also asked me to use a portable EKG (this is the one I have) to take a reading, if possible, during a time when my heart rate was especially high, and I was experiencing chest pain. She told me to email it to her personally so that she could see it right away, and gave me her email address. (Bonus, my doctor is married to a top cardiologist as well!)
THINGS GET REAL
Capturing that reading was pretty easy because it was happening a lot more frequently.
That evening, while I was brushing my teeth, I could feel my pulse start to race. I could hear my heart beat pounding in my ears, faster and faster. I glanced down at my smart watch (this is the one I own) and saw my heart rate steadily climbing. I grabbed the EKG monitor and took a reading. Although I wasn’t doing anything strenuous, my heart rate was now 165 beats per minute. My normal heart rate is around 60-ish.
I sat quietly for 5 minutes with my eyes closed and practiced slow, mindful breathing. I took another reading. It had dropped to 96 bpm, but was still way higher than it should be…and that was after five minutes of total relaxation.
Looking back, I think this was the point where I started to believe myself. That’s weird to say, but I was really beginning to doubt that there was truly anything wrong. All of the tests were coming back normal, and I was the only person who was saying something felt “off”. I had really started to think that maybe I was overreacting or making something a bigger deal out of this than it was.
There’s something about holding tangible proof in your hands that suddenly makes it all real, and those EKG readings were the first real thing I could give to my doctor so that she could see what was happening. I emailed it to her as requested, and at 7:30 the next morning, I got a call from the clinic saying I needed to go see the cardiologist.

FINALLY…A DIAGNOSIS
Over and over, I have said that I am extremely fortunate that I’ve been able to get doctor’s appointments scheduled quickly throughout this ordeal. It has been tiring to go back and forth to the hospital (about an hour away from where we live), but I am so grateful that I haven’t had to wait weeks or months to access care.
The cardiologist was able to see me the same week.
By the time I got to my appointment, I was feeling pretty lousy and extraordinarily fatigued. The tachycardia and shortness of breath were happening pretty much every time I tried to even stand up. It made no sense to me. I certainly have not gotten so out of shape that just standing up is considered physical exertion, have I??
He only had to examine me for about 20 minutes before he knew exactly what was wrong. He diagnosed me with Dysautonomia.
That’s a mouthful…let me break it down.
If you remember back to science class in school, we all have something called the Autonomic Nervous System. The ANS is responsible for doing all of the bodily tasks that we don’t think about…like, pump blood, digest food, sweat, dilate the pupils of our eyes, etc.
With dysautonomia, the ANS malfunctions in one or more ways. Science hasn’t figured out exactly why this happens yet, but they know that it can occur following a bad viral infection–just like what I had. They also know that there are several risk factors that might predispose a person, like having Celiac Disease–which I also have.
Technically speaking, dysautonomia isn’t a diagnosis in itself. Rather, it’s an umbrella term for a family of different diseases. There are at least 15 known diseases within the dysautonomia family, and the type I have is called Postural Orthostatic Tachycardia Syndrome (aka “POTS”).
Here’s what POTS means:
Postural – Related to the position of the body
Orthostatic – Standing up
Tachycardia – Heart rate above 100 bpm
Syndrome – A group of symptoms that consistently occur together
When a person stands up, gravity works on the body and, for a moment, the blood is pulled down toward the earth. The ANS–when functioning normally–kicks in and adjusts our circulatory system to pump the blood back up like it should.
For some reason, in people with POTS, there is a malfunction in the ANS. The circulatory system falters, and in an effort to compensate for the problem, the heart tries to pump faster and faster to make up for it and not allow us to pass out from lack of oxygen to the brain (although, that sometimes happens anyway).
Honestly, our bodies are freaking amazing, don’t you think? Even though things aren’t working right, I think it’s remarkable the way the body tries to override what’s not working to save us. Truly an amazingly resilient design!
HERE’S THE TOUGH PART
In addition to this being incredibly personal, one of the reasons I’ve delayed sharing the full details of what’s going on is because Rob and I are both still trying to work out our feelings about all of this. The most difficult thing about all of this is that there is no cure for this disease.
On top of that, I haven’t even reached a point where I’m stabilized yet. I’ve continued to acquire more of the characteristic symptoms each week, and we don’t know when that’s going to level off. We haven’t figured out the right medications, dosages, and treatments to control my symptoms yet, and my doctor has told me this is going to take a lot of patience on all our parts. She doesn’t even think we’re close to that place yet, and hopes we might be after another year.
That is a whole lot to digest at one time, on top of watching my body continue to fail me.
I am, without a doubt, navigating the stages of grief. Depending on what moment of the day you talk to me, I might be in one place or another in that grief process. That’s tough on my loved ones, and I feel guilty about that. I want to be upbeat and optimistic for them. I don’t want to give them a reason to worry about me. But sometimes I’m scared, discouraged, frustrated, stressed, angry, in denial…you name it, I feel it.
Right now, as I’m writing this, I’m crying. Typing all of this makes me feel incredibly raw. Rob just passed through the room on a phone call and saw me. He didn’t have to ask…he already knows that deciding to go through this journey publicly is hard for me, but also something I feel like I need to do. He paused for a minute to kiss my forehead, squeeze my shoulders, and then grabbed me a box of tissues.
Rob has been my rock through this. He’s handling everything, in every aspect of our lives right now–making meals, doing housework, keeping up with farm chores, handling all of our business stuff, driving me back and forth to appointments, pushing me in the wheelchair…literally everything is on his shoulders. I married a saint.

WHAT LIFE’S LIKE
Every week, I seem to acquire new and/or worsening symptoms that are characteristic of this disease. There is a spectrum of severity for POTS patients, and I keep reminding myself that things could be worse–and that, hopefully, things will eventually be better.
Right now, at the time of this writing, these are what I’m dealing with all day, every day. They are all due to the malfunction in how my circulatory system is moving blood around my body and to my organs.
Tachycardia and Chest Pain: Currently, standing up causes arrhythmia. So, I’m basically horizontal for the majority of the day. I just started a new medication that seems to be keeping me from getting too, too high up there. That’s given me a few-minutes-long window for standing up that makes it possible for me to walk to the bathroom, or to refill my water bottle. My heart rate still increases by way too much, but it gives me just a little sliver of time where I can stand without things getting completely out of control and causing massive chest pain. I’ve only been on this drug for 4 days, so that’s not enough time to tell what’s going to happen with this, but I’m hopeful. The last one we tried only lasted for 4 days before really bad things happened. I’m also wearing a heart monitor for the next two weeks (as shown in the photo above) so that my cardiologist can get some data about what happens throughout the day.
Shortness of Breath: This one technically goes along with the tachycardia, but since it’s painful in a different way, I gave it its own subheading in the list. The best way I can describe this is like trying to breath at a really high altitude. Even though I’m taking big breaths, I don’t feel like I’m filling my lungs. Sometimes it becomes so bad that I can’t talk because I’m breathless.
Dizzy and Lightheaded: This also happens whenever I stand, but also while seated upright. Lying down is the only way I can really keep this under control. I think of these symptoms as “annoying” since they aren’t actually painful, but they certainly wear on me throughout the day. These symptoms also make it very tough (and dangerous) for me to walk. I have to be holding onto something to get my bearings because everything feels like it’s spinning around me, and I get off-balance really quickly.
Cognitive Issues: I have two specific areas where I’m bothered in this area–memory and speech. I’m very forgetful, even in the middle of a conversation. I have trouble staying with what’s happening or what’s being said (even if I’m the one talking). I forget what I’m doing while I’m doing it, or what I’m talking about. And, on a similar note, I have trouble getting the words to my mouth. Even though I know what I want to say, I can’t get it to my lips. For example, this morning, I knew that I wanted to say the word “strainer”, but it wouldn’t come out of my mouth…so I said “the yellow thing”. And Rob knew what I meant! Usually, this manifests as just a delay…like, I’ll be talking and get to a word that isn’t coming and I just pause…and then it will get there. But sometimes I’ll use a replacement word, if I take too long and get frustrated. I’ve also noticed that I’ll type the same word several times in a row within a sentence, but I’m not even aware of it until I go back and re-read what I wrote.
Blurred Vision: I’ve worn glasses for over 20 years, but in the past few weeks, my eyesight has become super blurry. Again, without blood circulating properly, this is to be expected.
Fatigue: We’re all familiar with the heart rate chart posted on the workout equipment at the gym, right? Now, imagine that your heart rate is in those “high performance” exercise zones for hours upon hours a day. It is exhausting, to say the least. Add in the rest of the symptoms, the side effects of medications, and the overall stress of all this, and it is debilitating.
HOPE AND RADICAL ACCEPTANCE
Even though there is no cure for this illness, we’re still clinging to hope. With time, dedication, and a good team of doctors, it can be possible for many patients to find the right balance of treatments to manage their symptoms (albeit, with occasional flare ups). At the same time, there are people who can’t because of the severity. And, there are also people who go into remission, and their symptoms essentially disappear until something else triggers a relapse.
Right now, we don’t know which of those camps I’m going to be in.
I can tell you that I’m committed to doing everything I can to fight this disease. I want my life back. Yes, I know things are never going to be exactly the same again, but I certainly am going to give everything I can to work with what I’ve been given.
In our family, we practice radical acceptance. What this means in a nutshell is that instead of fighting against the water’s current, you flow with it. That doesn’t mean that you don’t try to change things about your life–not at all!–it simply means that you accept life with a healthy dose of reality, and you work from that place to achieve the life you want to live.
This applies to all areas of our life, and it takes a mindful effort to practice radical acceptance. It’s not something you perfect or master and just live happily ever after–it’s a way of living that guides us. We may veer from the path, but we keep learning, practicing, and growing with these ideas leading us.
The reality is, I have this illness. It comes with certain symptoms, and they’re part of my everyday life. My work, now, is to address those symptoms and try to improve my condition rather than ignore them and continue to live the way I used to, which will only make me feel worse because I’m working against what my body needs.
That means:
- Eating the right foods to nourish my body and tossing out those that don’t serve me (no matter how badly I might want them). Honestly, we already eat a fairly healthy diet. We’ve been vegan for decades, I don’t drink alcohol or consume caffeine, and I’m gluten-free to manage my Celiac Disease–so those recommendations are already checked off the list. But there are changes with this illness that might help me, like reducing simple carbs, cutting out sugar, increasing my salt intake (to try to increase the volume of blood in my body)–and I’m diligently doing all of those things. I’m also working on breaking up meals so that I eat 6 times a day. This works because it doesn’t require as much of the body’s blood to be needed by the digestive system. I find this especially challenging because I don’t like big meals to begin with and tend to have a small appetite, so in my pre-POTS life, I was much more likely to skip a meal than eat an extra one. So far, I’ve managed to bump myself up to four “meals”, and this week, I’m going to try adding a fifth. More on that later!
- Drinking a ton of water each day. One of the things that can help POTS patients is to try to increase their blood volume, which will basically force circulation to improve, and possibly re-train the ANS to function properly. The recommendation is to drink 2-3 liters of water per day, along with increasing salt intake. My doctor also instructed me to add electrolyte tablets to my water since that amount of water can wash away the minerals and good stuff that your body needs to function. Drinking that amount of water is really hard for me, but by golly, I’m doing it religiously.
- Allowing my body to rest. I will tell you quite candidly that this is, by far, the most difficult thing for me. I would much rather that the doctors gave me a list of all of the things I could go and actively do to feel better than to be told that I need to do nothing. That seems completely backwards to me. But the fact is, my body has been under a huge hardship for months, and it needs a break. I am trying so, so hard to do this to the best of my ability.
- Recharging the autonomic nervous system through meditation, yoga, mindfulness, and breathing exercises. I think I might need to write a whole other post just on this topic because it’s really fascinating how it works. I’ve practiced yoga and mediation for many years, but I’ve faltered lately. Now I’m working to get back into my routine. This means that I have to schedule and plan for this during the day so that I ensure it actually happens rather than getting caught up in a Netflix marathon or playing solitaire all day. (grin)
- Elevating the head of the bed. The theory here is that this helps to re-train the ANS to tolerate orthostasis (being vertical). We tried to do this last week, but failed miserably because our bed frame really isn’t conducive to this. A new attempt will be coming soon.
This is not an exhaustive list of what I’ve been told to try, and we’re working to correct as much as we can while not overloading ourselves to the point where we can’t manage all of the changes. One day at a time, we’re getting there–and that is really the whole point.
WHAT I REALLY WANT YOU TO KNOW
This is one of the longest blog posts I’ve written, especially considering it is a very intimate glimpse into our personal lives. I want to thank any of you who made it to this point because it shows that you care, and that means so much to us right now.
My intention is to continue openly sharing this chapter of our lives with you because I believe that there is strength in community. I also want my struggle to have an impact that’s greater than myself. If what I’m sharing here about my challenges can be of help to even one other person, then that would be the greatest gift I could hope for in this experience.
Finally, I hope that sharing my own struggle will help others to see that, when it comes to viruses–any virus, really–the options are not limited to “full recovery” versus “death”. People all around the world are suffering long term damage to internal organs beyond just the lungs, like the kidneys and brain, following COVID infections. This is why it is so, so, so important to take this issue seriously.
I never knew that something like this could happen following a viral illness. And I certainly never thought something like this would happen to me. Now, I will have this disease for the rest of my life.
Please–I implore you–stay home unless you have an essential reason to go out. And by “essential”, I mean ask yourself what is really worth it if it meant you might die or have to live with a lifelong disability in exchange for that choice. When it’s necessary to go out, wear a mask, practice social distancing of at least six feet, and maintain proper hand hygiene.
I wouldn’t wish this experience on anyone.











Kristi~ I am so sorry to hear this! I’m glad you were able to get diagnosed rather quickly.
I, also, have dysautonomia and agree it is hard to describe what your body is going through!
I like your meaning of radical acceptance!
Best wishes on finding your new balance!❤️
I've recently had all the same hospital test you mentioned here. So far everything is normal. I did NOT have covid or any viral infection. My symptoms are extreme fatigue, shortness of breath and dizzizness. I'm very overweight and 68 years old. One other thing. You are so lucky to have a supportive husband. Unfortunately, I do not have that. God Bless you. Will be keeping you in my prayers.
Thank you for sharing. I have learned a lot from this. Prayers for you and your husband. Remember, we are all here caring about you and the Lord above will hold you in His arms through this.
Thanks for sharing your experiences. I hope that this goes away, or at least gets better, as quickly as it came on. The body is a magical thing. Get well and my thoughts are with you.
Thanks for sharing your experiences. I hope that this goes away, or at least gets better, as quickly as it came on. The body is a magical thing. Get well and my thoughts are with you.
Blessings on this difficult 🙏 journey. Hope your Resting and may you endure your illness with hope and faith ..